Here are three ways to describe what “death with dignity” is for people at the end of their lives – as well as for caregivers who love them, work with them, and support them in different ways.
If you are wondering about the line between prolonging life and saying to a doctor, “Let my loved one go”, you might be interested in reading Knocking on Heaven’s Door: The Path to a Better Way of Death by Katy Butler. It’s part memoir, part medical history, and part spiritual guide. It’s a book that explores what dying with dignity means in today’s health care system.
For this article, I conducted a brief email interview about end of life care and death with dignity with Robert W. Lehmberg, MD, FACS is an Assistant Professor of Hospice and Palliative Medicine at the University of Arkansas for Medical Sciences. Here, he shares his thoughts on dying with dignity as well as end of life care in general.
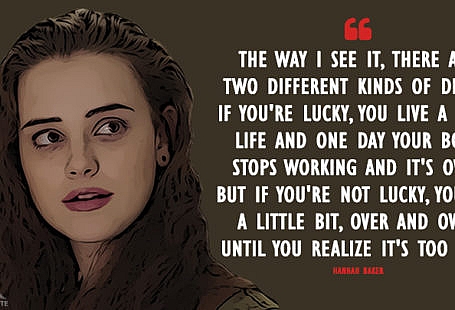
“I think the phrase, ‘death with dignity’ for most people means they get to tell their story and share what they have accomplished in their life,” says Dr Lehmberg. “Death with dignity means reviewing their life, knowing it was worthwhile, and sharing their legacies.” He adds that death with dignity means not dying in pain and not dying alone. It’s also about realizing the importance of letting people tell their story about their life and experiences.
Death With Dignity
Here are Dr Lehmberg’s thoughts on dying with dignity, in his own words. If you are nearing the end of your life – or you work with palliative patients in a hospice or other setting – you might want to read When You’re Scared to Die. As Dr Lehmberg says below, fearing death is normal and accepting death is an important step towards dying well.
Dying “well” often includes a life review. When I first started working in hospice care with palliative patients, I thought dying people were more concerned with what was going on now and what would happen in the future. I didn’t realize that doing a life review is a very important part of dying with dignity.
Everyone deals with death differently. I encounter different kinds of people, some who know they are dying and some who don’t. Some are relieved to talk about it with a physician, and some really do not want to talk about it at all. Learning what death with dignity is involves knowing what the dying person wants, and who he or she is.
Acceptance of death is important in achieving peace. The “war” and “sports” language and analogies in healthcare (“lost the battle with cancer,” “he’ll beat this, he’s a fighter”) is unhelpful because it creates a win-lose situation in which peace and God’s will seem secondary.
One of the most important qualities for a palliative physician (or anyone who wants to know how to be with a dying person) is to be comfortable with death. Learn how to talk and listen without experiencing discomfort yourself. Being comfortable with death allows you to focus on the dying person, not your own feelings of anxiety or fear.
Death once-in-a-lifetime experience. For each individual and family, end of life care and dying is a unique experience. While I may work with palliative patients and see death a dozen times a week or on a daily basis, for the patient it is once-in-a-lifetime experience. For the family, death is a memory they will carry with them always.
Emotional and spiritual peace is crucial, but sometimes elusive. What I pray for, on behalf of my patients and myself, is peace. As a physician, I can take care of pain and treat anxiety. Everyone is scared – that’s normal, no matter how strong your belief. Emotional and spiritual peace is important and can be elusive for some. It is ideal to see a person die at peace. Many families have some conflict within. Being at the end of life offers an opportunity for family members and friends to come together and achieve peace for the person who is dying. Peace for the death itself, and for the dying person to know they are leaving with their loved ones in peace. That is what death with dignity is.
About death with dignity, you might be surprised to learn that palliative care – started early enough in the disease course – can actually extend the survival period. You may already know that hospice and palliative care improves quality of life of people with a terminal condition (read Alternative Therapies for Hospice Patients to learn more), but good quality hospice or palliative care can help people live longer.
What I want to say to dying people is you’re not going to be alone, you’re not going to be in pain, and you’re not going to be helpless. Working with palliative patients, and focusing on death with dignity, reminds me how important it is to be at peace with your life. Decide what is important to you, and what you value. Live for your values. I wish I had experienced the death of a loved one when I first started working in palliative and hospice care, so I could have had more personal insight. My initial experience of death – and death with dignity – was all clinical. I had never had a friend or family member die and been there with them. The process leading up to death is valuable, as is the death itself. If you have any questions or thoughts on death with dignity, please comment below.